References
Distraction osteogenesis part 2: technical aspects
From Volume 11, Issue 2, April 2018 | Pages 46-54
Article

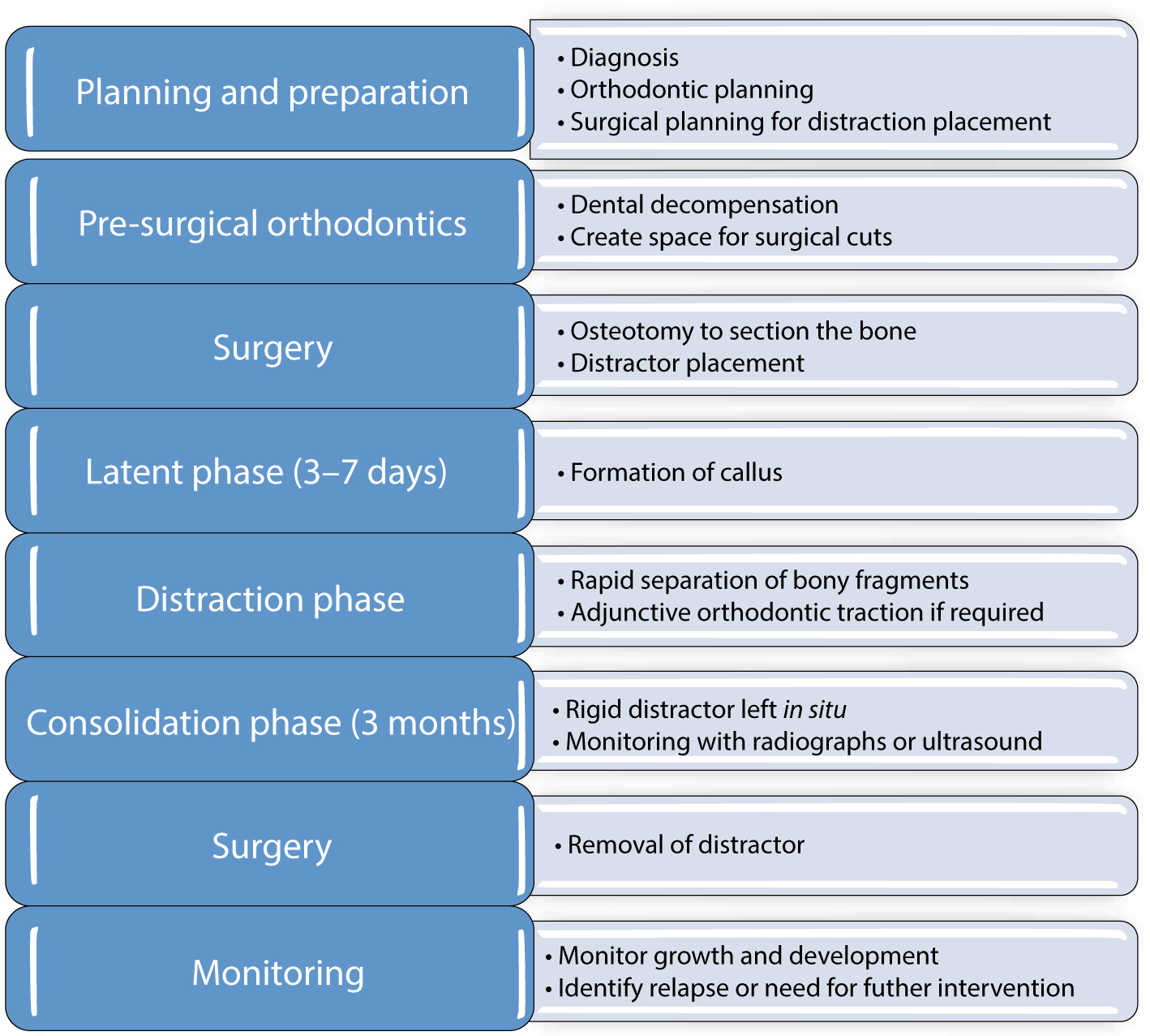
Distraction osteogenesis is undertaken in a number of key stages (Figure 1). The success of DO relies on meticulous planning and provision of care with input from a multidisciplinary team specialized in the craniofacial region.
Planning
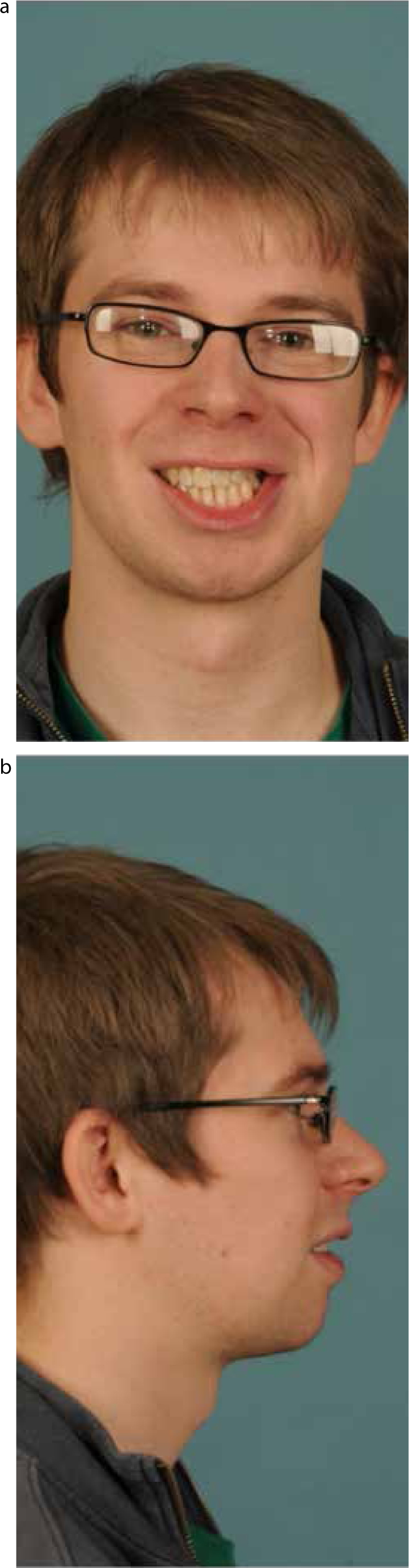
The first stage in DO focuses on planning and preparation. Identifying which structure is abnormal and the likely aetiology is essential to successful management. DO is used to correct the underdevelopment associated with hypoplastic or absent structures, to compensate for overdevelopment of contralateral structures. Diagnosing which structures require intervention is fundamental to planning the type, direction and magnitude of distraction.
A combination of photographs, conventional radiographs, such as orthopantomographs and lateral cephalograms, and 3D images are used for diagnosis and treatment planning (Figure 2). Advances in 3D printing from CBCT images has enabled the production of highly accurate 3D models of the craniofacial hard tissues, known as stereolithographic models, which are built up in layers from a polymer (Figure 3). Stereolithographic models can be used to aid visualization for diagnosis and for counselling patients. Detailed surgical planning and mock-distractor placement can be undertaken on models and used to produce a surgical stent that then accurately transfers the planning to the patient.1 The mock-up can also guide preparatory bending of distractors, reducing surgery time.2


Pre-surgical orthodontics
The aim of pre-surgical orthodontics is to produce an occlusion that can help guide the skeletal distraction and produce a stable occlusion. Much like preparation for conventional orthognathic surgery, the orthodontic tooth movement may include levelling and aligning, decompensation and co-ordination of the arches, with the aim of positioning the teeth in the ideal position in the basal bone. Fixed appliances are most commonly used due to their ability to control tooth movement accurately in all planes (Figure 4). Supplementary appliances, such as a Quadhelix appliance, may be required to gain maxillary arch expansion. If osteotomy cuts are planned in tooth-bearing regions, pre-distraction divergence of the roots may be necessary.3
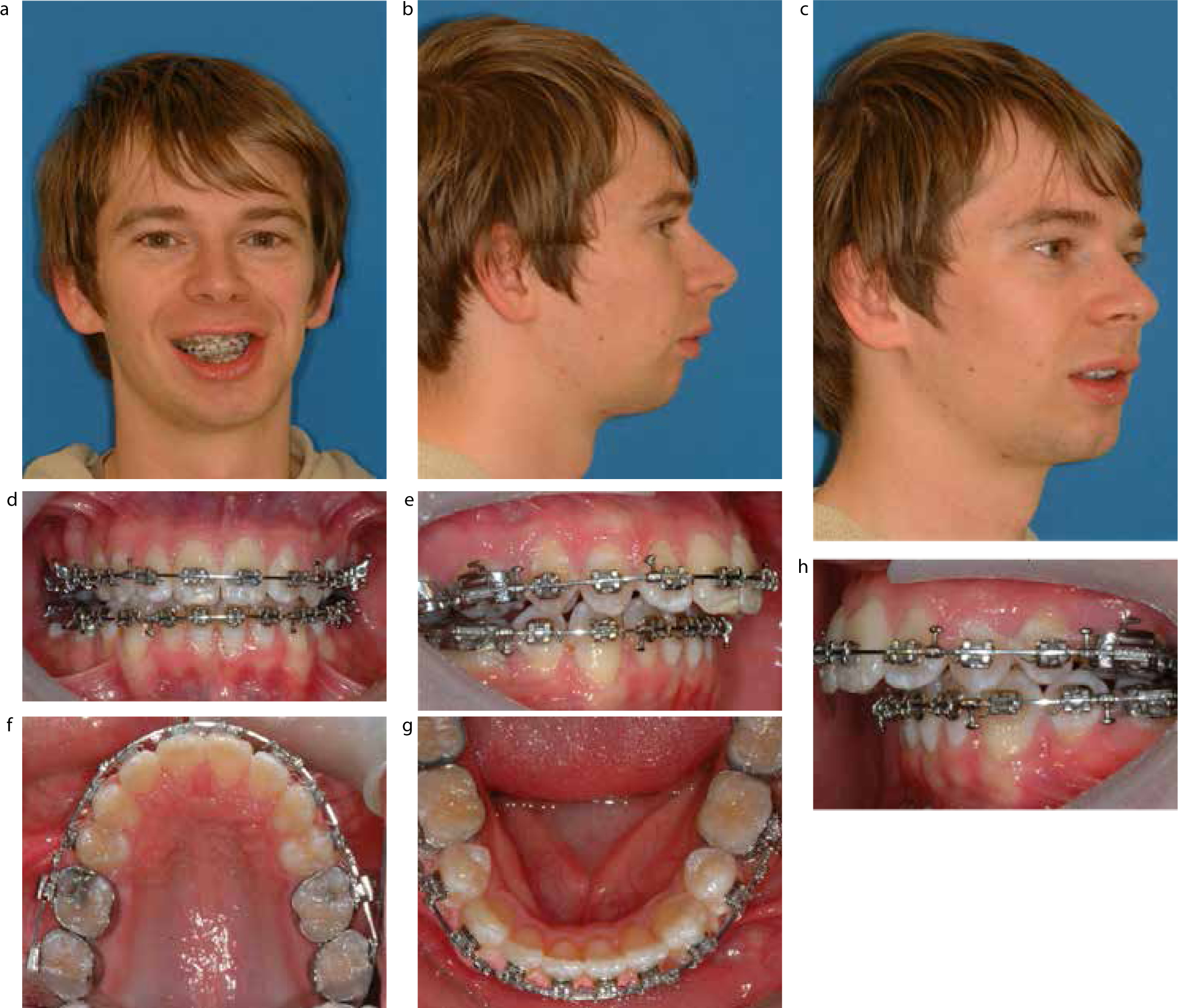
The fixed appliances are left in place during the distraction phase with passive stainless steel archwires. This provides a method for attaching inter-arch elastic traction during the distraction and consolidation phases. However, if the distraction will result in intra-arch expansion, the fixed appliances must be sectioned or carefully monitored and regularly adjusted to prevent interferences to arch lengthening.
In younger patients with craniofacial discrepancies who are undergoing DO as an interceptive measure to attempt to normalize growth and development, orthodontic treatment may not be necessary at the time of distraction. In these patients there is often a significant malocclusion, but orthodontic treatment is prohibited by the difficulties of planning orthodontic treatment and attaching a fixed appliance in the primary and mixed dentitions. In these patients DO is planned at a time to maximize the skeletal benefit, and correction of the occlusal discrepancies is postponed until the permanent dentition is established. Alternatively, a hybrid functional appliance is sometimes used.
Pre-distraction surgery
The preliminary surgical procedure has two purposes; to section the bone and place the distractor (Figure 5). The bone is sectioned in the optimum position and direction to allow separation of the fragments in the desired vector. Although DO of long bones usually involves a corticotomy, where the external compact bone is sectioned while maintaining the medullary cortex and periosteum, in the craniofacial region an osteotomy is usually accepted due to the narrowness of the bones. Intra-oral surgical access is preferred, where possible, to minimize scarring in mandibular and maxillary procedures. However, this can significantly limit access and consequently an extra-oral approach is often more appropriate.
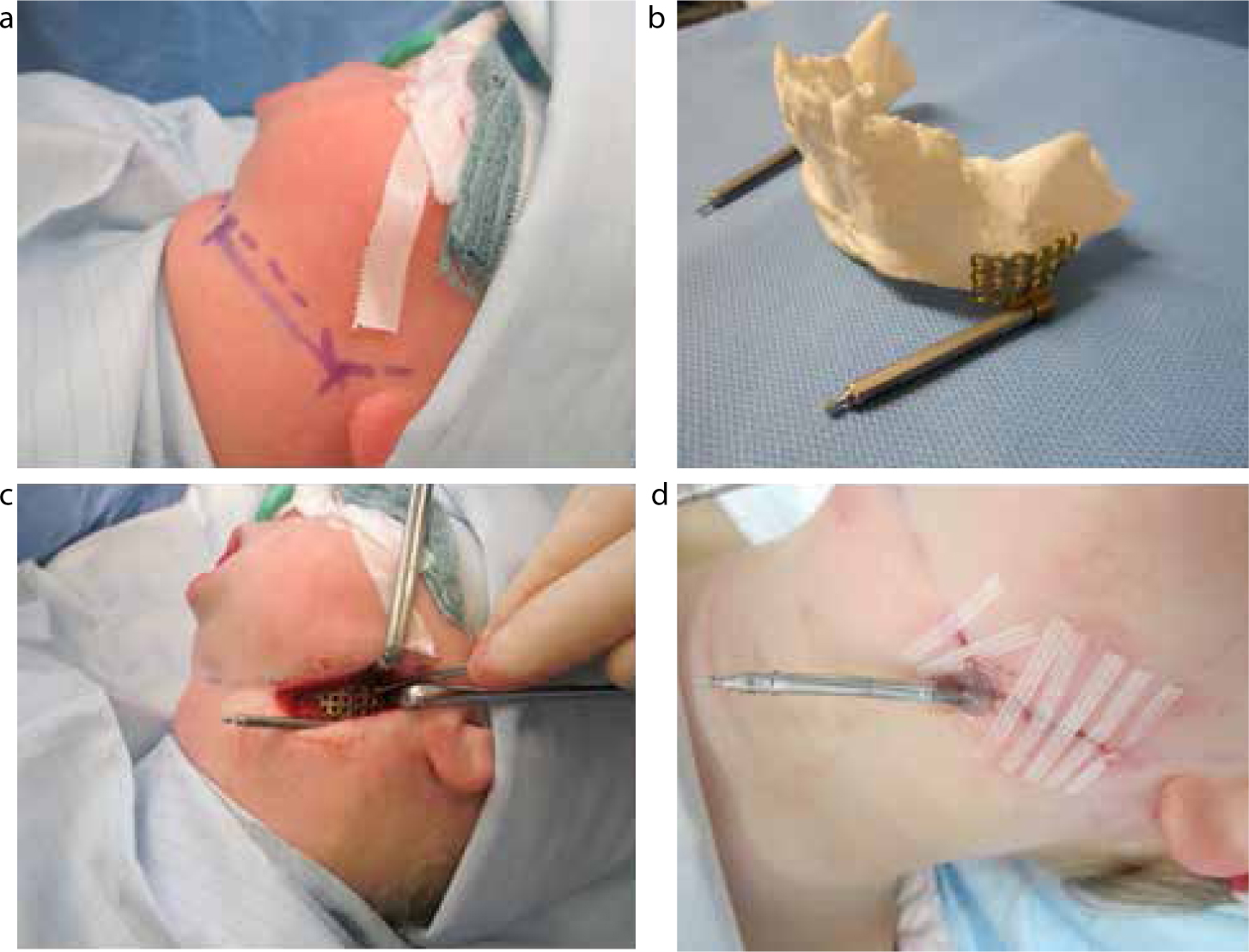
Placement of the distractor determines the vector of expansion and is therefore critical. During surgery, placement and securing of the distractor before the final surgical cut and osteotomy is performed ensures optimum positioning. This, in conjunction with meticulous surgical planning, optimizes the chance of a favourable outcome.
Types of distractors
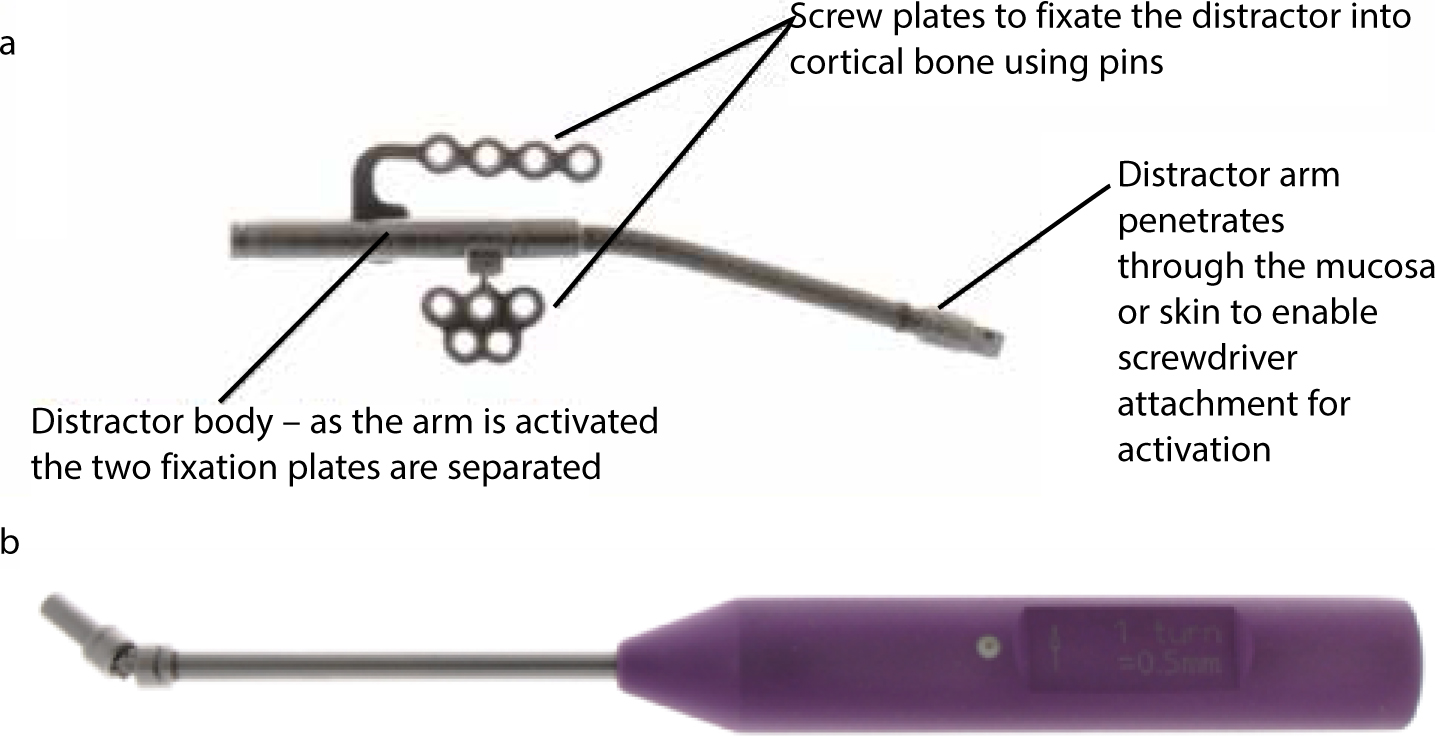
Distractors are manufactured from a lightweight titanium alloy or surgical steel and must be rigid enough to prevent distortion and flexing in the distraction site. A number of designs are available to suit different functions and are categorized as internal or external (Table 1). External devices attach to the bone through percutaneous pins that attach externally to fixation clamps. These fixation clamps are attached to distraction rods which, when activated, push the bony segments apart. Internal distractors can attach to either the bone, above or below the mucosa, or to teeth.4 Internal distractors are preferable in terms of social acceptability and to minimize scarring, but inadequate access for placement can limit their feasibility. The distractor components and different designs of distractor are illustrated in Figure 6.
| Internal | External | |
|---|---|---|
| Direction | Univector |
|
| Mode of attachment | Tooth-borne |
Bone-borne |
| Method of placement | Subcutaneous |
Subcutaneous |
Success has been demonstrated with bioresorbable mandibular distraction devices in babies with Pierre-Robin, eliminating the need for further surgery for distractor removal.5 A further area of great interest is the development of automated distractors employing motor-driven, spring-mediated or hydraulically-powered methods to allow remote activation and monitoring.6 This removes the need for patients to self-activate the distractor, potentially leading to improved outcomes.
Activation of the distractor
Following the initial surgery, a 3−7 day latent phase is given prior to commencing activation (Figure 7). The length of the latency period depends on individual patient factors, such as age, which will influence the speed of callus formation. The surgery results in a small gap, approximately 1.0 mm, in which a callus begins to form during the latent phase. This fibrous tissue consists of longitudinally oriented collagen with spindle-shaped fibroblasts within a mesenchymal matrix of undifferentiated cells.7
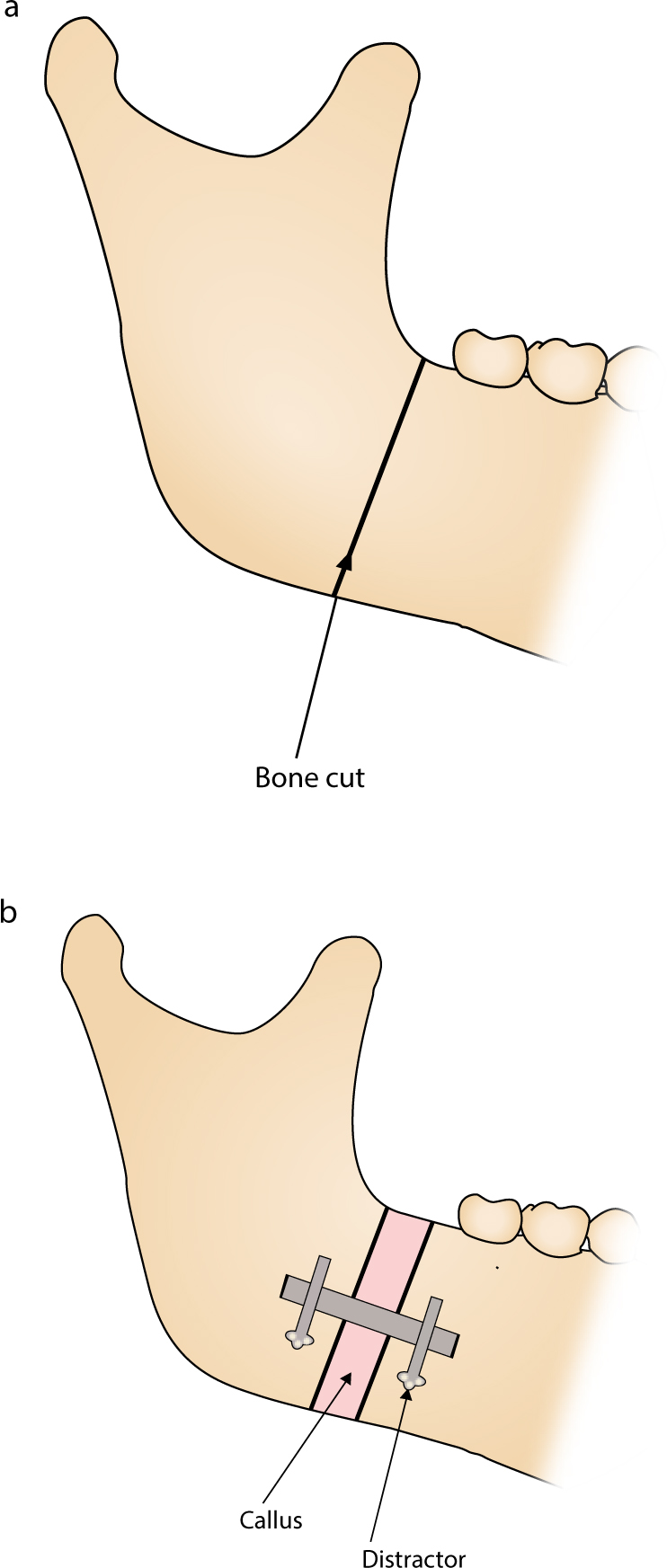
The distraction phase commences with the first turn of the distractor device and is continued until the desirable increase in bone length has been achieved. Controlled, incremental stretching of the callus through regular activation of the distractor initiates bone formation. Calcification of the callus begins as soon as distraction ceases and the rate and rhythm of distraction is therefore key; excessive activation of the distractor can cause poor healing, with elongation and thinning of the callus, while delay in activation will risk premature calcification of the callus and limited further movement. Age influences the ideal rate of distraction as younger patients grow faster. Specific distraction schedules vary but generally distraction is accomplished at a rate of two 0.5 mm turns per day, resulting in 1 mm distraction per day.
Clear information and communication with the patient and family is paramount for achieving a successful outcome. Activation tends to be completed by the patient or a family member at home following training from the clinical team. This can be a difficult task and motivation and compliance are essential.
If a large movement is being achieved with distraction, then the callus can tend to become thinned as it is stretched over a long distance. A process described as ‘pumping the regenerate’ may be carried out to prevent this. The patient is asked to turn his/her activation screw alternately forwards and then backwards to prevent calcification and allowing more callus to develop. Pumping the regenerate technique is also used in bilateral cases where one side requires more movement than another, such as in asymmetry cases. During the activation phase close clinical assessment is critical to assess growth and movement.
Post-distraction phase
The rigid distractor is left in situ during the consolidation phase to allow the callus to calcify and transform into haversian bone. This rigidity prevents movement of the segments of bone and newly formed callus that would cause fibrous union. Bony healing is monitored clinically and with regular radiographic examination (Figure 8). More recently, ultrasound has been shown to be an effective method for monitoring bone calcification, reducing the number of radiographic exposures required.8

During the distraction and consolidation phases, orthodontic traction can be used to guide the tooth-bearing regions and mould the regenerate into the ideal post-distraction position. Inter-arch elastic traction can be used with an antero-posterior, vertical or transverse vector to correct Class II or Class III discrepancies, reduce open bites or correct cross bites and cants.3
At the end of the consolidation phase, once adequate bone healing is evident, the distractor is removed. The patient is reviewed long term to monitor further growth and continued assessment of function and aesthetics. Orthodontic retention is provided to maintain post-distraction tooth positions (Figure 9).
Treatment timing
Unlike conventional orthognathic surgery where growth cessation is required prior to surgery, DO can be used in growing patients. This is based on the rationale that DO is largely used to manage underdevelopment of structures to optimize the potential for normal growth and reduce the complexity of future treatment. While DO can compensate for underdevelopment of bony structures, distraction does not result in a normal rate of growth post-operatively. A study evaluating mandibular growth after DO in children under 48 months of age with congenital mandibular hypoplasia showed that growth on the affected side remains less than that on the normal side.9 Similarly, distraction of the midface in Apert's and Crouzon's syndrome has been shown to have little effect on follow-up growth.10 Patients and families must therefore be warned that DO in childhood is not guaranteed to eliminate the need for further surgery. The timing of intervention is determined through longitudinal monitoring of development and informed decision-making between the clinical team and family about when it is best to intervene. The benefits of early intervention for normalizing development must be weighed against the impact of the procedure on the patient and family and the risk of relapse and repeat procedures.
Distraction osteogenesis is also used in non-growing patients where conventional orthognathic methods are judged to be unsuitable or have poor prognosis. In these patients, timing has little impact on the outcome from treatment and scheduling is therefore based on timing of patient presentation, patient wishes and service factors.
Potential complications
Improved soft tissue adaption and a corresponding reduction in relapse have been cited as major advantages of DO.11 A systematic review including six craniofacial DO studies, with a minimum follow-up period of 3 years, found that, although early relapse was seen up to 3 years post-distraction, the long-term stability of DO was generally good. The underlying cause of relapse is thought to be similar to that of orthognathic surgery, with soft tissue contraction playing a large part. The reviews authors did highlight methodological limitations in the included studies and the general lack of good quality evidence regarding long-term stability.12
Other complications of DO can arise during the surgical stage, during activation of the distractor or in the post-distraction period (Table 2).13,14
| Timing | Complications |
|---|---|
| Intra-operative | Incomplete bone fracture |
| Intra-distraction | Patient compliance activating the distractor |
| Post-distraction | Malunion or failure of callus to heal |
The team approach
Distraction osteogenesis is a complex procedure that relies on team members with complementary skills working together effectively to achieve the best possible outcome for the patient. Unlike cleft lip and palate management, the care pathway for craniofacial deformity care has not been formalized and the team composition differs across the UK. Standardization of care is complicated due to low patient numbers and the highly variable presentation of skeletal anomalies between patients. Although desirable, it is not always possible to have healthcare professionals with expertise in craniofacial nursing, speech and language, diet and psychology. In the absence of a designated DO team, patient needs should be assessed early and every effort made to formulate a holistic approach to management.
Diagnosis and planning tend to be undertaken by the Maxillofacial Surgeon and the Orthodontist together. Successful planning requires understanding of the abnormal anatomy and likely future growth, and the scope and limitations of any potential distraction. Orthodontists can provide input at the planning stage about how surgery and distraction can be optimized with pre- and post-distraction orthodontics.
Nursing staff familiar with craniofacial anomalies and the specific techniques associated with DO are invaluable in providing advice and support for patients. For example, some of the burden of training patients and carers to activate the distractor and reviewing progress in the activation period may be lessened by the judicious use of a trained nurse.
The psychological impact of DO has been highlighted by a randomized controlled trial that compared maxillary advancement with DO and conventional orthognathic surgery in cleft lip and palate patients. It was found that DO caused higher levels of distress, lower self-esteem and higher social avoidance in the peri-operative and immediate post-operative period. After the distractors were removed, the psychological parameters improved to show similar results to orthognathic surgery, and 2 years post-operatively the DO patients were more satisfied with their lives.15 Consequently, it is generally advised that any patients who have not already been given psychological support through attendance at craniofacial clinics should be offered ongoing support.
Although the incremental changes produced by DO might be expected to have less effect on speech than a single large move from conventional orthognathic surgery, the evidence is poor.16 One small study found maxillary advancement by distraction has a similar risk for velopharyngeal insufficiency in cleft patients as a single Le Fort I advancement.17 Similarly, an evaluation of speech changes after mandibular distraction in patients with hemifacial microsomia found a temporary deterioration in articulation and nasal resonance.18 For this reason, a speech assessment and expert advice is recommended for all patients being considered for DO.
Finally, input from a dietitian may be desirable to help patients maintain sufficient nutritional intake before, during and after treatment. Difficulties in eating can arise from a limited masticatory ability caused by the original craniofacial abnormality or by treatment. Satisfactory nourishment improves post-operative recovery and consideration should be given to dietary supplements, if indicated.
