Article

The decision was made to extract all four first molars and to carry out upper and lower fixed appliance therapy.
Treatment involved upper and lower fixed appliances, 0.022 x 028” MBT straight wire system with anchorage reinforcement of the upper second molars using a transpalatal arch with large Nance button. This is essential because the anchorage obtained from upper second molars is insufficient to correct a Class II buccal segment occlusion. The upper second molars should not be allowed to move forwards until the lower second molars have been mesialized to a Class I relationship and the canine relationship has improved.
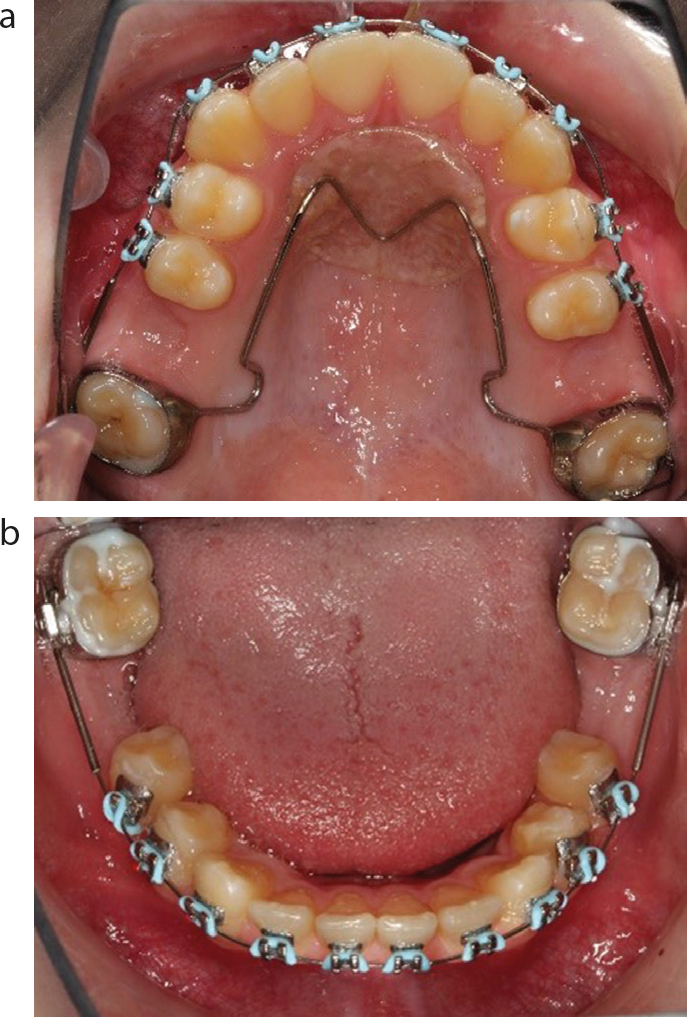
Initial aligning archwires (0.014 Nitinol) were placed with stainless steel tubing protecting the long flexible spans and the archwires were cinched back (Figure 1) The latter not only prevents the lengthening of the arch by incisor proclination, but prevents the flexible wire being displaced from the molar tube during mastication and subsequent fracture of the wire. Repeated flexing of the wire results in the wire hardening, which then leads to its fracture. Short segments of NiTi wire can be ingested, and there have been reports of patients needing abdominal surgery to recover these small wire fragments.1
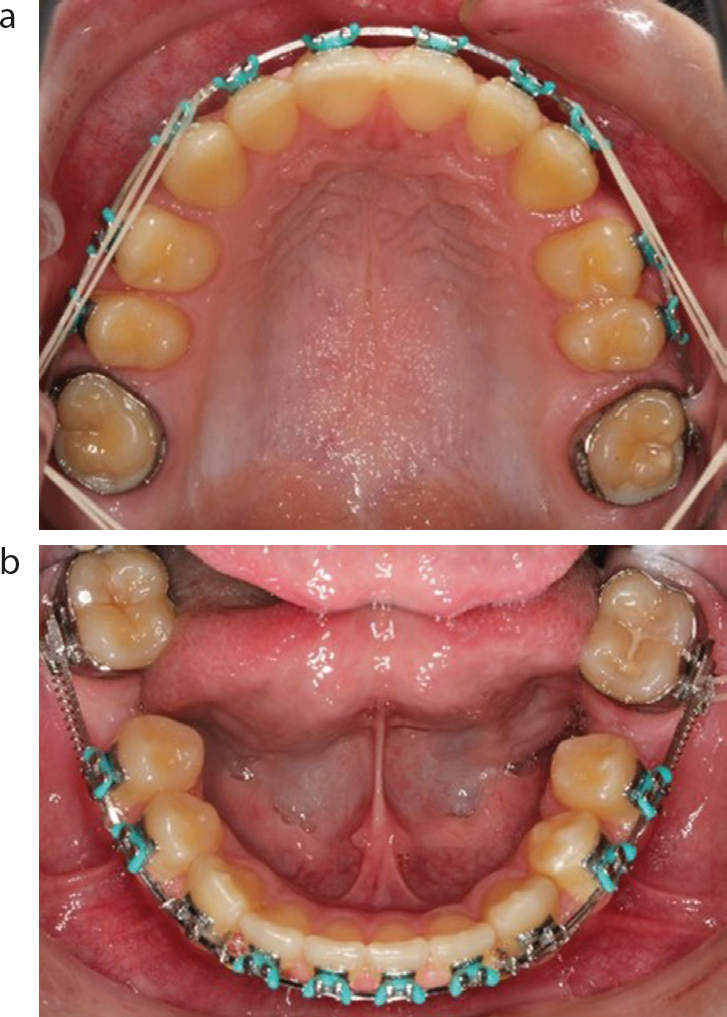
We progressed through 0.018 x 0.025” NiTi, to 0.019 x 0.025” steel with soldered hooks (Figure 2). The TPA can be removed near end of space closure when anchorage can be supported with inter-arch elastics. Figure 3 shows the end of treatment following 21 months of fixed appliance therapy. Unfortunately, elastic wear was not as successful as hoped, and the patient had a 2–3 mm Class II buccal segment on the right.
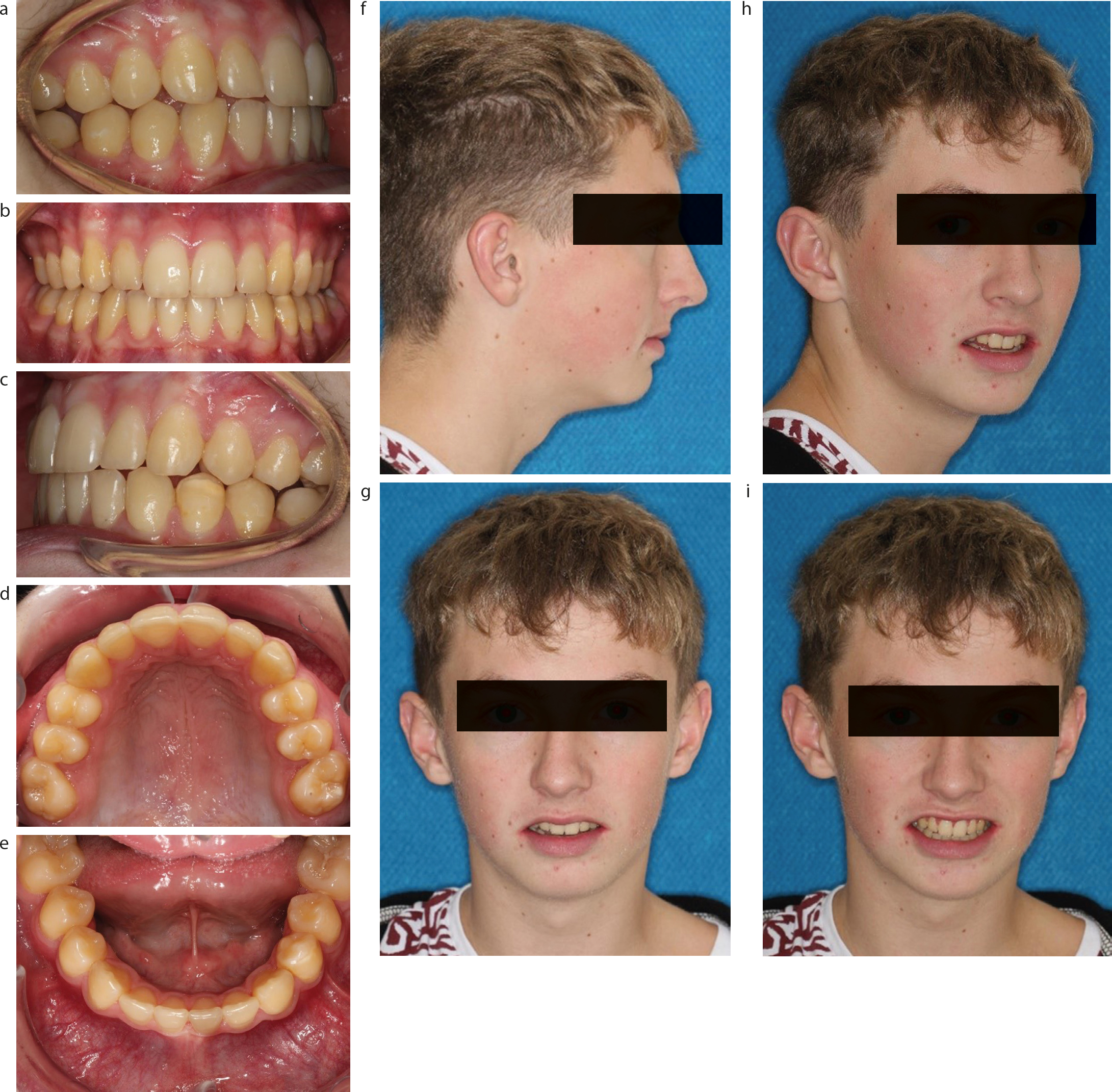
The final issue was whether the third molars would erupt into a good position because this is unpredictable. Often, teeth that look to be in an impossible position, move favourably and others in a classically ‘perfect position’ to erupt, sometimes do not. The patient was advised that if the third molars came through in a poor position, he would be offered more orthodontic treatment to upright them. The upper third molars and the lower right third molar erupted well. There was a slight impaction of the lower left third molar where the mesial marginal ridge was 2 mm gingival than would be ideal. Remedial treatment was discussed, but the patient felt he had an acceptable result and declined further intervention.
Is there a higher risk of caries in this situation? As we have all seen, in cases of impaction of lower second or third molars, carious lesions can result. This patient would appear to be at low risk; however, he has been warned that there is a risk of food packing leading to caries and has been instructed to stick to a healthy low sugar diet and to maintain good oral hygiene in the future.
Regular radiographic review with the dentist should also be advised as distal surface caries in the L7s can be asymptomatic until advanced and possibly unrestorable.
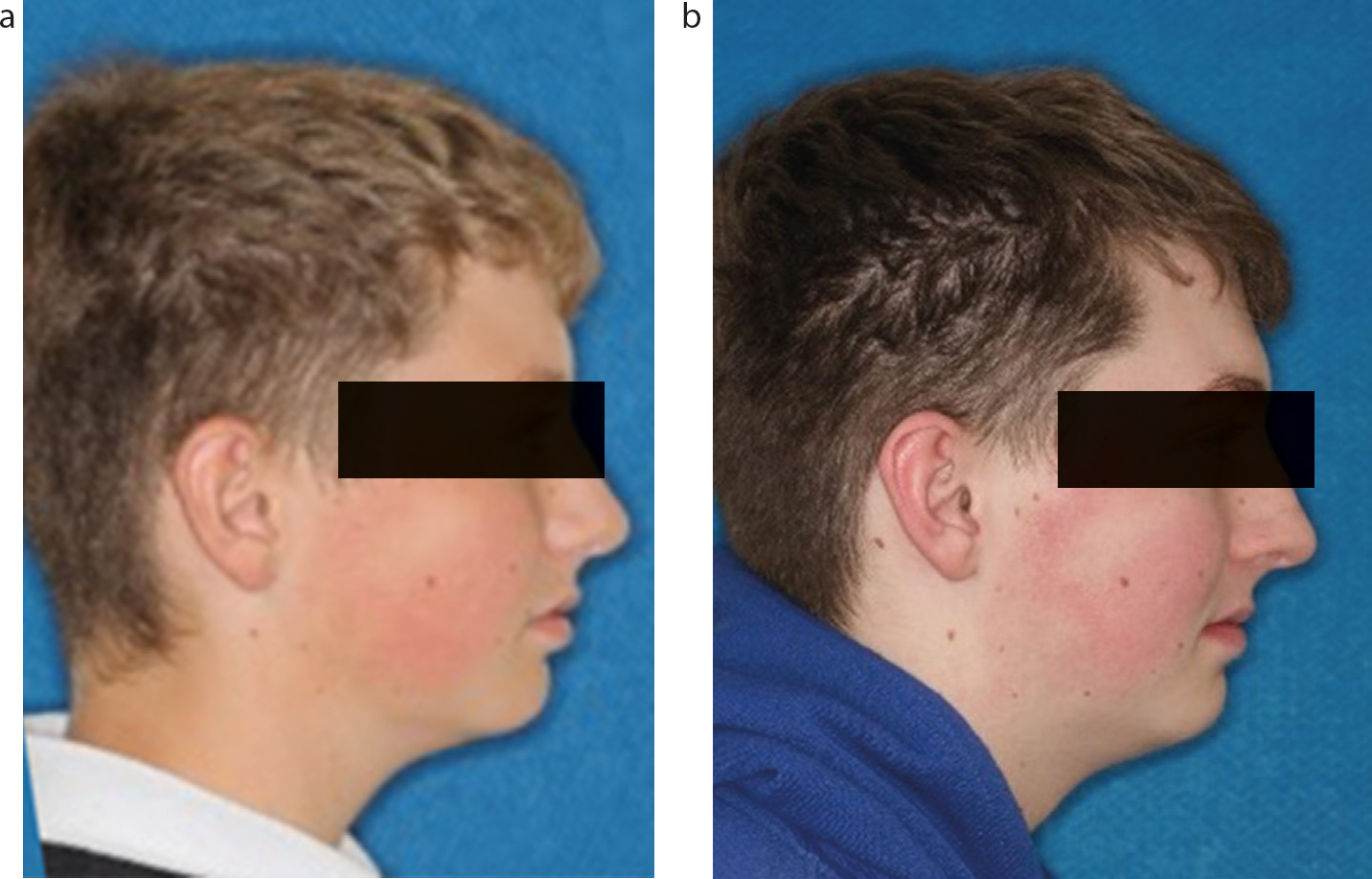
Figure 5 compares the pre and post-treatment facial profile from the start of treatment to the eruption of the third molars (3 years 9 months after the start of treatment). The small increase in naso-labial angle is noted and was one of the few findings comparing extraction and non-extraction Class I orthodontic patients by Frietas et al.3

Only time will tell, but he currently has an unrestored dentition, which should last him many years.
