Abstract
Pain is a common side-effect of orthodontic treatment. The aetiology of orthodontic pain, pain pathways and pain management will be described.
From Volume 13, Issue 2, April 2020 | Pages 50-56
Pain is a common side-effect of orthodontic treatment. The aetiology of orthodontic pain, pain pathways and pain management will be described.

Pain and discomfort have been reported to be experienced by up to 95% of orthodontic patients1,2 and can be felt at all stages of treatment. This includes early interceptive extractions,3 the placement of separators,2,4 bands,2 archwires2,5,6,7,8,9 and, finally, at debond and retainer fit.10,11 This pain can affect a patient's quality of life in a variety of ways and has been suggested as one of the principal barriers to orthodontic treatment.12 A survey of the pain experienced by 116 adolescent patients during orthodontic treatment13 found that orthodontists routinely underestimate the level of pain caused by their treatments. Indeed, the pain experienced following archwire placement is believed to be greater than that experienced following extractions.6 It is therefore important that orthodontists understand orthodontic pain in order to improve pain management, patient acceptance, compliance and overall satisfaction with orthodontic treatment.
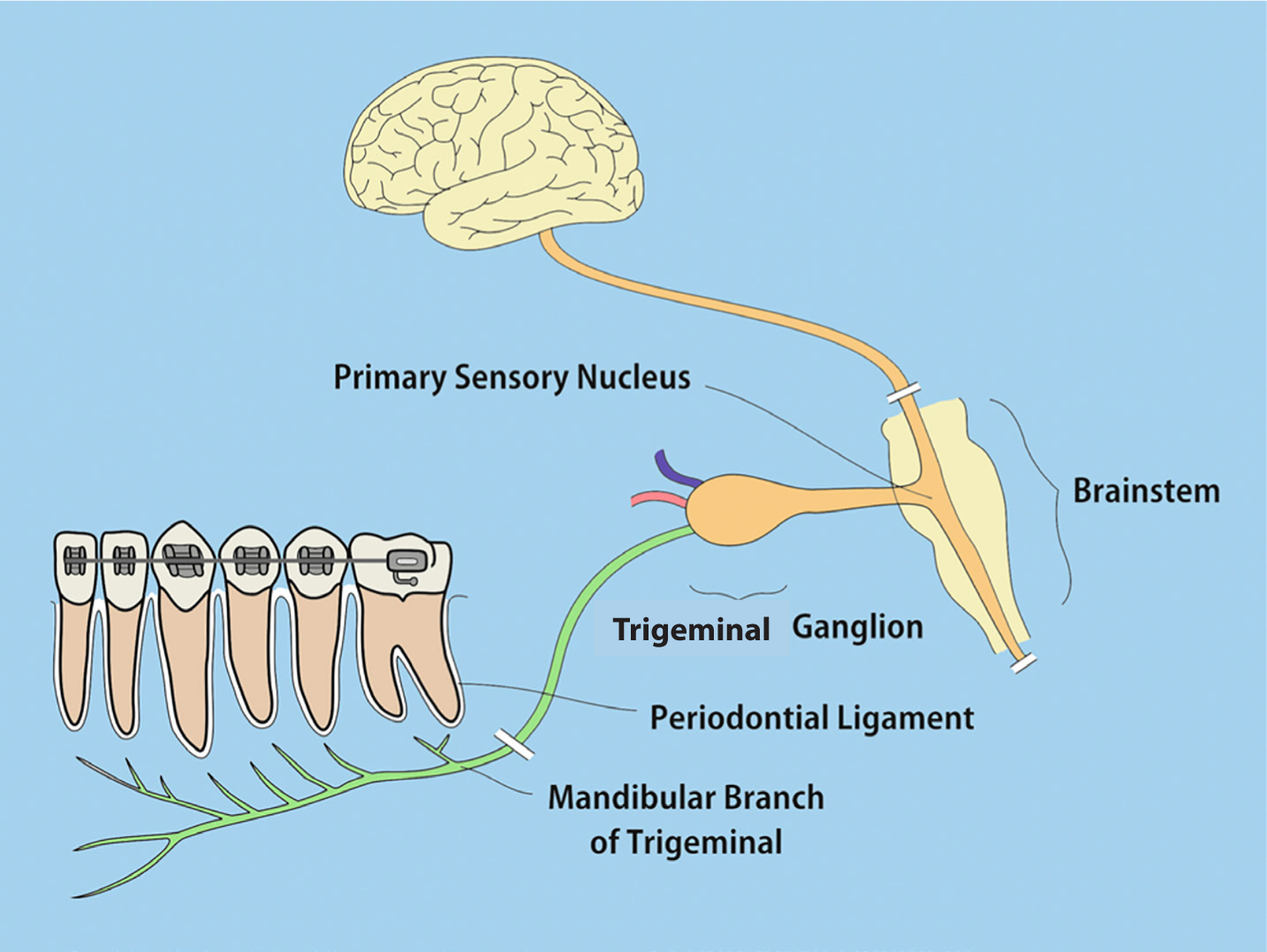
The sensation of pain is initiated in one of two ways, either by the direct stimulation of nociceptive nerve fibres by a mechanical, chemical or thermal stimulus; or indirect stimulation following the release of any one of a number of inflammatory mediators, including histamine, bradykinin, substance P, prostaglandins and serotonin. These mediators are released as a result of tissue injury. Once stimulated, nociceptive fibres undergo depolarization and, in the case of orthodontics, the sensation of pain is transmitted from the pulp and/or periodontium to the central nervous system via nociceptive afferent fibres. These are mainly lightly myelinated primary afferent Aδ fibres, which respond to mechanical or thermal stimulae and are associated with acute pain. The slower primary afferent unmyelinated C fibres respond to mechanical, thermal or chemical stimulant and are associated with a slower, persistant pain. These primary afferent nociceptive fibres are those of the trigeminal nerve, whose cell bodies lie within the Gasserian or trigeminal ganglion (Figure 1).
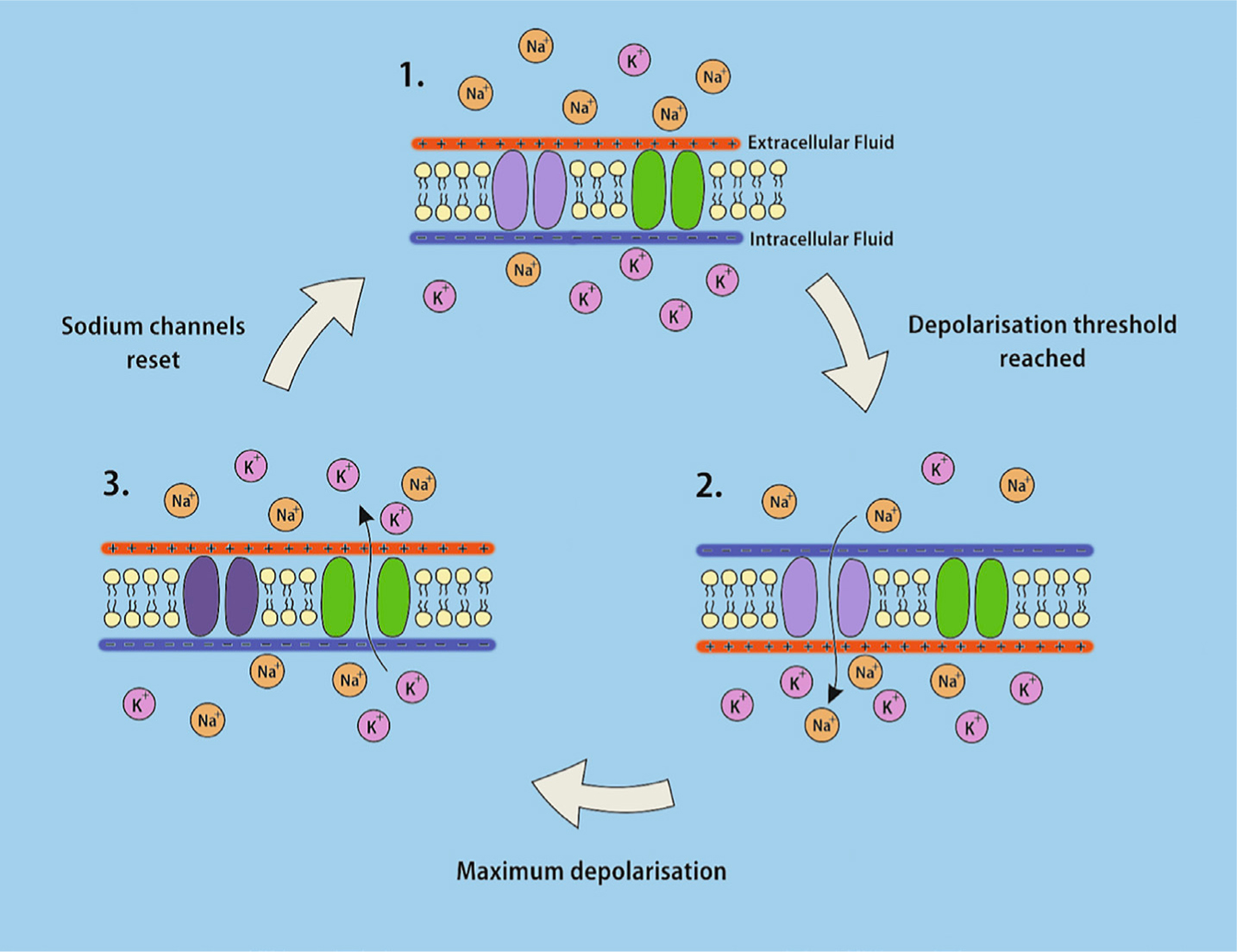
Once initiated, the pain stimulus is transmitted along the neuron axon by propagation of an action potential. At rest a neuron axon is negatively charged intracellularly (-70 mV) relative to the area surrounding the neuron. Action potential propagation is caused by the activation of voltage-gated sodium channels in response to depolarization of the neighbouring axon segment. This leads to a rapid influx of positively charged sodium ions into the cell along a concentration gradient. This reverses the polarity in that segment of the axon. The polarity is then reinstated by the sodium channels entering an inactive state, halting further ion flow, and the opening of voltage-gated potassium channels that allow positively charged potassium ions to flow out of the axon down their concentration gradient. Each segment depolarizing triggers further voltage-gated sodium channels to activate downstream and the action potential cascades along the axon. In myelinated Aδ fibres, the axon is surrounded by a series of Schwann cells that electrically insulate the axon. There are spaces between the Schwann cells called nodes of Ranvier. The action potential jumps from node to node down the axon length significantly speeding up conduction (Figure 2).14
The degree of pain experienced by individuals in response to an identical noxious stimulus can vary greatly from person to person.15 The perception of pain may be influenced by a number of different factors. Anxiety has been shown to be a factor affecting dental pain, lowering the reported threshold9 and increasing the likelihood of the avoidance of dental treatment.15 It is therefore important that the level of anxiety associated with orthodontic treatment is minimized in order to optimize the patient care experience.
It has also been suggested that both age and gender might have an effect on perceived orthodontic pain, but the results of studies investigating these factors are somewhat equivocal. While some studies have demonstrated age has no effect,8,9 others have found the level of pain reported by adolescents to be greater than in other age groups.2,16 Similarly, the evidence for the effect of gender on pain perception is mixed. At the time of appliance or separator placement, two studies have reported pain experience to be greater in girls than in boys,4,16 whilst others have concluded that gender has no effect on pain perception following the placement of initial archwires.5,8,9
It is generally considered that orthodontic pain starts at around 2 hours after appliance placement, with some studies reporting that this is the case for between 91% and 97% of orthodontic patients.4,16 It then usually peaks at 24 hours5 before gradually subsiding over the next 5 to 7 days.7,8 Interestingly, it would seem that up to 25% of orthodontic patients report experiencing pain for longer than 7 days.16
A number of investigations have been carried out to determine which sites within the dental arch experience the most pain during orthodontic treatment. In almost all cases, the teeth which experience the most significant pain are the incisors, in particular the lower incisors, and this is the case during both initial alignment and at debond.5,10,11,16,17
In recent years a number of studies have considered the possible effect of both bracket and wire type on reported pain. In particular, comparing self-ligating brackets with conventional brackets, which utilize elastomeric ligation (Figure 3). Perhaps due to the complex and also subjective nature of pain, the effect of bracket type is not conclusive. Some studies report less pain when using self-ligating brackets,9 others report greater pain with self-ligating brackets, but only during insertion or removal of the archwire,7 and others report no difference at all between the two bracket types.8

There have also been a number of investigations into the pain experienced with lingual versus labial fixed appliances. It would seem that the pain related to the teeth and the periodontium is most probably the same, but what is different is the site of any soft tissue-related discomfort, which unsurprisingly is usually greater in the tongue in the case of lingual brackets, and greater in the lips and cheeks in the case of labial brackets.18 A recent systematic review and meta-analysis concluded that, overall, there is more oral discomfort experienced with lingual appliances.19
With respect to archwire choice and pain, a recent Cochrane review has found no evidence that the use of any particular type of wire for initial alignment has any effect on perceived pain.20
Debonding requires the removal of the brackets and bands at the completion of treatment, along with residual adhesive from the enamel surfaces of the teeth. The most commonly used method of bracket removal is to use debonding pliers (Figure 4).2 In the case of metal brackets, this works by the pliers distorting the bracket base, leading to crack propagation and either cohesive failure within the bonding material, or adhesive failure at the interface between the bonding material and the bracket base or enamel surface. Care needs to be taken to make this process as pain free and efficient as possible. The risk of damage to the enamel is greater in the case of the removal of ceramic brackets because both the bracket material and enamel are relatively brittle. The pliers must therefore initiate crack propagation within the bonding material, or at its interface with the bracket base or enamel surface. With both metal and ceramic brackets, pain may be experienced if forces are transmitted to the teeth, particularly rotational or torqueing forces. Alternative methods of debonding, such as the use of thermal and laser instruments, have been investigated, but to date there is little evidence to indicate whether their use is associated with any more or less pain at debond.

Although there are a considerable number of studies centred on the pain associated with orthodontic procedures, such as separator placement and archwire placement, there is limited research on the pain associated with debonding. A study in Iowa, USA, assessed patient discomfort levels at debond and found that a threshold force existed above which discomfort and pain was felt.10 The level of this threshold was not uniform throughout the mouth and was significantly influenced by tooth mobility and the direction of any force applied. Intrusive forces were the best tolerated by patients and with the rather surprisingly high mean threshold being 934 g. This study also reported that pain varied according to the teeth being debonded. The mandibular incisors were found to display the greatest pain at debond, with a mean discomfort threshold of below 830 g. However, it should be noted that this study only involved 15 patients and pain was assessed in 16 teeth per patient (first premolar to first premolar). No data were provided for pain experienced in the molar regions.
A larger randomized controlled trial11 assessed pain at debond in 90 subjects, half of which were biting on a soft acrylic wafer during debond. It showed similar results to the Iowa study, in that the lower anterior teeth were deemed to be the most painful by patients. This study also reported that subjects who bit on an acrylic wafer during the debond process reported reduced pain levels in the posterior dentition. This may have been due to the intrusive forces applied to the teeth during biting. From the raw data it would seem that 93% of the patients experienced some degree of pain during debond. Although the sample size was reasonably large, the power calculation was based on research around clinically significant pain reduction within an accident and emergency setting21 for acute pain, which may not translate well to pain in orthodontic patients.
The management of pain during orthodontic treatment has been an important area of research and numerous studies have looked at the use of analgesics during procedures, such as separator22,23,24,25,26,27,28,29,30 and archwire placement.31,32,33 Although most studies have focused on the use of ibuprofen or paracetamol to relieve orthodontic pain, other studies have looked at alternative analgesics. These have included naproxen,32,33 piroxicam22 and aspirin.28,33
In addition to the type of analgesic, there has also been some debate as to the timing of providing analgesia in order to reduce orthodontic pain and discomfort. Although post-operative analgesia would be expected to reduce pain, it has been suggested that pre-emptive analgesia may also be beneficial. When Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), such as ibuprofen, are given pre-operatively, it has been suggested that it can reduce the inflammatory response as the body has a chance to absorb and distribute the medicament before the onset of any tissue damage and prostaglandin production.34 One study into pre-emptive analgesia24 assessed the effectiveness of pre- and post-operative ibuprofen in 51 subjects and found that pre-emptive ibuprofen, given an hour before separator placement, significantly reduced the level of pain reported 6 hours post-operatively and later at bedtime. Interestingly, no significant difference in pain was found between those in the placebo group and those that only had post-operative ibuprofen. However, this may have been due to the fact that the post separator ibuprofen was administered at 3 and 7 hours after separator placement, rather than immediately after placement. Other studies investigating pre-emptive administration of ibuprofen at separator placement26,27 support these findings, and it has been suggested that the decrease in observed pain is as a result of the pre-emptive anti-inflammatory effect of ibuprofen, rather than its analgesic action.
A number of studies have compared ibuprofen and paracetamol in orthodontic pain management.23,25,28,30,31,33 Bradley et al compared paracetamol to ibuprofen in a non-inferiority randomized trial of 159 patients and found that ibuprofen was superior in providing pain relief.30 The ibuprofen group reported less pain at most intervals from day 1 onwards. Whilst other studies on separator placement have supported these findings of the superiority of ibuprofen over paracetamol,23,28 others have shown no significant difference between the two.25,31 However, these results need to be interpreted with some caution, as three studies25,28,31 used a lower 600−650 mg dose of paracetamol rather than the more usual clinical dose of 1000 mg.
It has been suggested that the use of NSAIDs might slow orthodontic tooth movement. This is because the rate of tooth movement is linked to bone remodelling which ‘involves a complex cascade of events and agents that act synergistically and antagonistically’,35 including interleukins and prostaglandins. The use of NSAIDs may have a negative effect via inhibition of some of these pathways and therefore on tooth movement.36 More specifically, altered remodelling of the vasculature and extracellular matrix may occur due to inhibition of Cyclooxygenases37 involved in prostaglandin synthesis by the NSAID. However, to date there is no evidence to suggest a clinically significant effect of NSAID use on orthodontic tooth movement in humans. This is probably because their use for pain relief is very transient during such treatment.
A number of non-pharmacological methods have been suggested to control orthodontic pain, including electrical stimulation (Transcutaneous Electrical Nerve Stimulation (TENS) machines),38,39 tooth vibration,40 cognitive behavioural therapy,41 bite wafers42,43 and text message follow-up.44 Some of these methods are more practical for clinical use than others.
A randomized controlled trial,45 which assessed pain control after initial archwire placement, compared a placebo group with a group who received cognitive behavioural therapy and a group who received ibuprofen at 6, 12 and 24 hours post archwire placement. The results demonstrated that cognitive behaviour therapy significantly reduced pain perception, and was comparable to that seen with patients who received ibuprofen post treatment. However, as we have already seen, it is pre-emptive ibuprofen, rather than post-treatment, which has been shown to be most effective24,26,27 in terms of pain management.
In recent years, there has been an interest in the use of bite wafers or chewing gum for pain relief. It has been postulated that chewing on something hard, immediately after adjustment of an orthodontic appliance, helps loosen tightly grouped periodontal fibres, which in turn reduces oedema and inflammation by restoring the lymphatic and vascular circulation.43
However, the effectiveness of bite wafers in orthodontic pain management would seem to be somewhat equivocal. In a study of 49 patients,42 the participants were given either a bite wafer or told to take over the counter (OTC) medication, post initial archwire placement. It was reported that the pattern and level of pain was similar in both groups, with the bite wafers being at least as effective as OTC medications. By contrast, Otasevic et al found that biting on wafers increased the level of pain to a greater level than in those patients that were merely instructed not to eat hard foods for 7 days post wire placement.43
Orthodontists commonly advise their patients to avoid chewing gum in case it damages the orthodontic appliance. However, a recently published large randomized controlled trial involving 1000, 11−17 year-old patients undergoing fixed appliance therapy found no evidence that sugar-free chewing gum use leads to more appliance breakages. What chewing gum use did lead to, however, was a small reduction in the amount of ibuprofen used following both the initial bond up and the first archwire change.46
In conclusion, pain may be experienced during all of the stages of orthodontic treatment with fixed appliances, with up to 95% of patients being impacted. Pain is very subjective in nature and the experience of pain can differ considerably from one individual to the next, for the same procedure. Pre-emptive analgesics, such as ibuprofen or paracetamol, are worthwhile, as is the use of post-operative sugar-free chewing gum.
The identification and management of orthodontic pain is important in order to improve the acceptance of orthodontic treatment, patient compliance and overall satisfaction with the final outcome.