References
Multidisciplinary Treatment – A Case Report
From Volume 12, Issue 1, January 2019 | Pages 13-16
Article

Hypodontia is the term used for the developmental absence of one or more teeth, excluding third molars. The prevalence of hypodontia in the primary dentition is 0.1%−0.9% and in the permanent dentition is 3.5%−6.5%.1 In Caucasian populations the third molars are the most commonly missing teeth, followed by the second premolars and then lateral incisors.1
Management of hypodontia cases is often difficult and complex, particularly in patients that have been severely affected. Delivery of a suitable holistic treatment care pathway for these patients requires the expertise of various specialists forming a multidisciplinary team. Treatment planning for congenitally missing teeth should be based upon a comprehensive evaluation of a patient's age, his/her occlusion and the specific space requirements, as well as the size and shape and morphology of adjacent teeth. Integrated care is best provided through an experienced team of clinicians from a range of specialties, working together in a hypodontia clinic. This method of treatment is considered to be the gold standard for the clinical care of this very special group of patients.2
Hypodontia patients are commonly associated with spacing in the dental arches. Generally, the treatment options for missing lateral incisors are space closure or space opening and maintenance for prosthetic replacement.3 The decision between space closure and space opening usually requires consideration of many factors including:
Autotransplantation is defined as the transplantation of embedded, impacted or erupted teeth from one site into extraction sites or surgically prepared sockets in the same person. Autotransplantation provides a viable and predictable treatment option, with its goal similar to that of a dental implant: to replace a missing or non-restorable tooth and provide increased function and improved aesthetics. Success rates have been reported of up to 90%.4
Indications for transplantation include congenitally missing teeth as well as traumatized or ectopically positioned teeth, particularly when there is overcrowding involving premolars elsewhere in the mouth. The benefit of transplantation of a tooth with incompletely formed roots is that it offers the chance of maintaining tooth vitality. Transplantation also enhances the chance of maintenance and preservation of alveolar bone volume by physiological stimulation of the periodontal ligament.5,6 Dental implants in younger adolescent patients are contraindicated because the implant and the bone fuse as part of the osseointegration process, thus preventing further eruption of the implanted tooth, in comparison to the adjacent teeth which keep developing vertically. If implants are placed before facial growth has largely ceased then a step in the vertical heights is almost inevitable.
Significant factors that influence success of autotransplantation include: patient selection, age, health status, dental status and caries risk, oral hygiene, root development and finally surgical technique.
The sequence of autotransplantation procedure is:
This treatment sequence clearly highlights the need for specialists in at least four different dental disciplines, emphasizing the need for excellent lines of communication between all the specialties to ensure the most efficient and effective multidisciplinary management.
This case report aims to illustrate multidisciplinary care and show the clinical application of autotransplantation in a severe hypodontia case, as well as demonstrating the benefits of space opening for the provision of single dental implants.
Case report
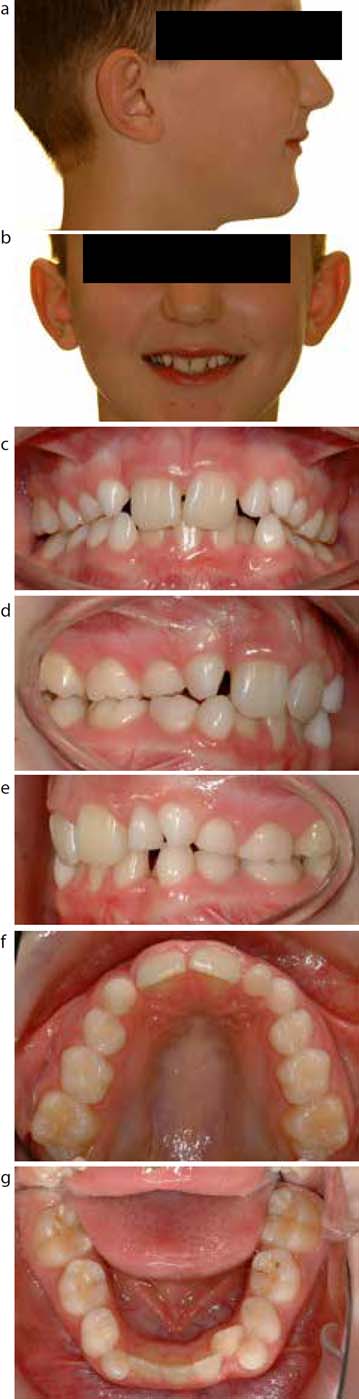
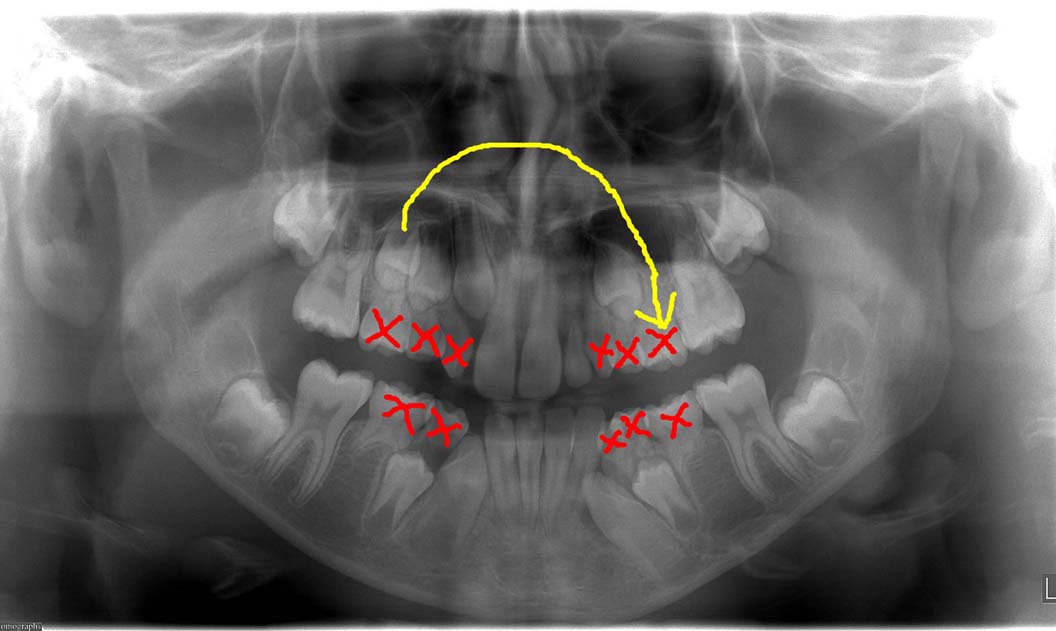
A medically fit and healthy 10-year-old Caucasian male attended the orthodontic clinic at Royal Chesterfield hospital following referral from his general dental practitioner. He presented with a Class II division 2 incisor relationship, on a mild Class II skeletal base with an increased FMPA and complicated by severe hypodontia (Figures 1a−g). The OPT radiograph confirmed the congenital absence of UR2, UL2, UL3, UL5, LR5 and LL5, with the third molars yet to develop.
The patient's problem list comprised:
The diagnosis and treatment planning for this case was discussed initially by the orthodontists and restorative dentists at the joint hypodontia clinic at Chesterfield Royal Hospital. Further consultations were had with the maxillofacial surgeons.
The management of this complex case was as follows:
It was decided that the patient would benefit from having his UR5 transplanted to the UL5 site to provide an extra dental unit in the upper left quadrant. The UR5 was transplanted when its root was only partially formed and the tooth had a significantly open apex to maximize the chances of success. Following transplantation the tooth was splinted for 10–12 days (Figure 3).
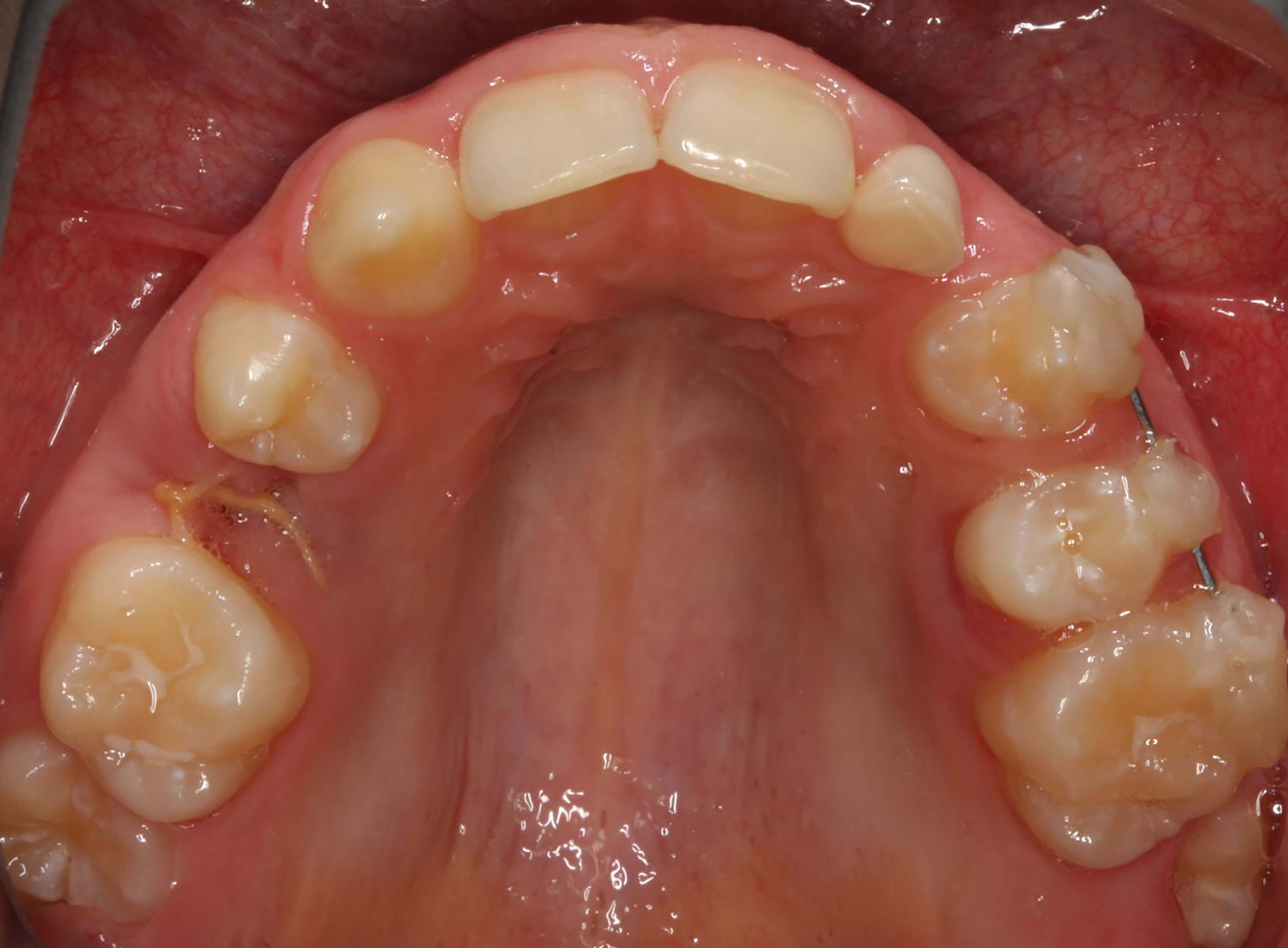
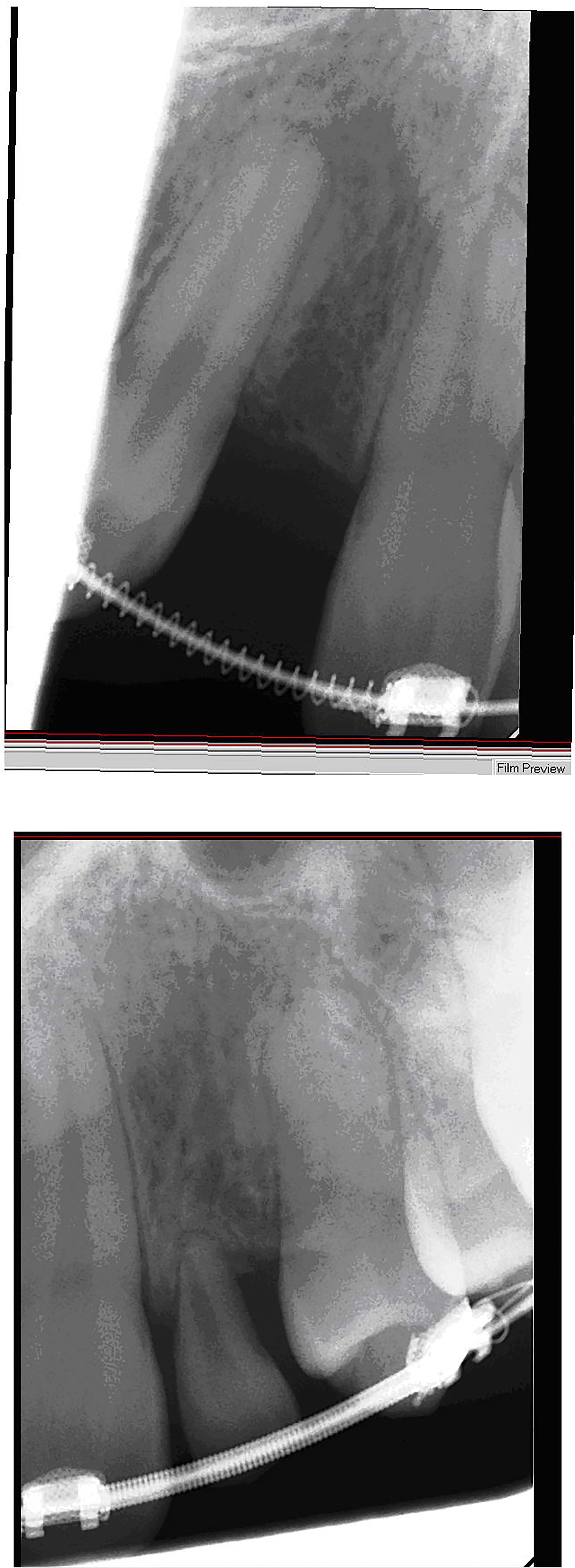
Orthodontic treatment was delayed for 12 months to allow complete recovery of all the tissues following the surgical trauma. By this time the premolar had revascularized successfully and root formation continued to the normal level. OPT to demonstrate eruption of all teeth and continued development of transplanted premolar ‘UL5’ (Figure 4).

A definitive course of fixed appliance therapy was carried out including treatment on the transplanted premolar (Figure 5), and it took nearly 36 months to correct the malocclusion fully (Figures 6a and b). After lengthy consultation with the restorative dentists, the upper right lateral incisor space was reopened to allow placement of an osseointegrated implant and the ULB was finally extracted to allow an implant to be placed. Prior to debond, periapical radiographs were taken and passed by the implant team to ensure that they were happy with the positions of the teeth adjacent to the implant site (Figures 7a and b). The osseointegrated implants were left in situ for 3−6 months to integrate fully (Figure 8) before placement of the final restorations. Throughout the retention period it is essential to prevent any relapse, which may jeopardize the final restoration placement. This is often done with Essix retainers which contain prosthetic teeth, to restore dental aesthetics fully, thus encouraging patients to comply with wear protocols (Figure 9).




From the initial referral, this complex treatment plan took 9 years to complete the transplantation, the definitive orthodontics and then place the osseointegrated implants. This process required meticulous planning involving orthodontists, restorative dentists and oral surgeons. The patient attended 10 joint clinic appointments over the course of his treatment which involved 36 appointments at Chesterfield Hospital.
Discussion
Treatment staging is extremely important in this case owing to the delicate nature of the transplantation of UR5. Meticulous planning is required to ensure correct timing of transplantation to maximize the possibility of an uneventful recovery. Ideally, the donor tooth has to revascularize fully and root development needs to continue before the appropriate commencement of orthodontic treatment.
Transplantation in this case was successfully carried out when the patient was 13 years old. The open root apex of UR5 enabled revascularization to occur. The disadvantage of this early approach involving transplantation, when dealing with these complex hypodontia cases, includes the prolonged retention which is always required after orthodontic treatment, until the patient is ready for implants. This retention period of course relies on good patient compliance as inadequate retention, after orthodontic treatment, can rule out the possibility of dental implants, either if crown alignment has not been maintained or if the roots have been allowed to encroach upon the potential implant site.
In cases such as these after discussion between the orthodontists, the restorative dentists and the implantologists, there could well be a requirement for further complex orthodontic treatment prior to implant placement.
The generous separation of roots, adjacent to potential implant sites, to allow adequate space for risk-free placement requires a very enthusiastic and co-operative patient. Oral hygiene and diet need to be exemplary throughout the whole treatment period to minimize the possibility of demineralization of the teeth. Regular appointments with a hygienist or dental health educator are frequently recommended.
Summary
Treatment in this case has involved a lengthy course of surgical, orthodontic and restorative treatment, including 10 visits to multidisciplinary clinics with multiple consultants present at each visit. Over 9 years of treatment was required leading up to the placement of dental implants.
In a patient with severe hypodontia with missing multiple units in each quadrant, this type of prolonged and expensive multidisciplinary treatment is certainly justified. In patients with less severe hypodontia the placement of adhesive bridges might be considered as a less expensive and less time consuming alternative.
All hypodontia patients should be referred by their general dental practitioners to a multidisciplinary clinic to allow an experienced team of professionals to discuss the alternative treatment options, therefore enabling both patient and parents to make an informed decision on future care.
